This article was originally published in Yoga Journal. Read the full article here.
There’s only one window in the hospital room. It doesn’t open, but it stretches nearly the entire length of the wall, from built-in bench to ceiling, inviting light into the otherwise stark space. A large treble clef sculpture centers a modest fountain in the courtyard outside. On one of San Diego’s classic unseasonably warm April mornings, the air catches and carries the dancing water droplets to the ground. Inside, an orchestral performance of a different sort unfolds.
Here, in the COVID unit of Sharp Memorial Hospital, mechanical whirring replaces the string section, pumping medical devices sub for the woodwinds, and a sharp, irregular intake of crackling breath establishes the bass rhythm. This last instrument belongs to Vernon, a man in his 60s who was diagnosed with COVID-19 two weeks prior. Tubes in his nostrils meet in a V under his chin where they flow to the oxygen tank sitting at his side. His eyes are closed, his maskless face relaxed, hospital sock–adorned feet planted evenly on the ground as he sits in front of the window, the treble clef fountain at his back.
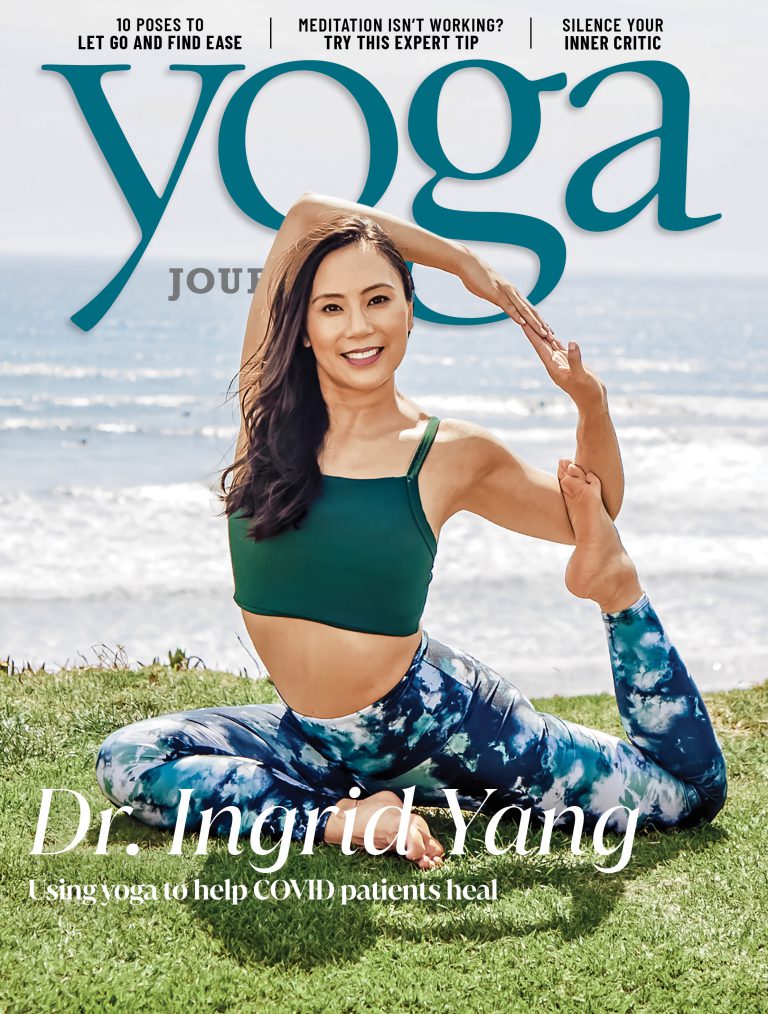
Knee to knee with Vernon sits hospitalist-physician Ingrid Yang, MD. Her hands gracefully carve the space between her and Vernon, gesturing as she conducts a symphony of yoga therapy. “We’re going to inhale through the nose, three, two, one,” she says, drawing her hands slowly upward as together she and Vernon expand chest and belly. “Hold for a count of three, two, one. Exhale through pursed lips—try to depress, use the contraction of the diaphragm—that’s nice.”
There’s a musicality to Yang’s presence, from her bell-clear voice and cadence of speech to the rhythmic way she moves through the world. A trained Reiki healer, she’s a master of shifting energy—almost visibly sculpting it at all times, knowingly or not. She gestures continuously as she speaks, leading Vernon through a pranayama-based protocol she developed that’s so simple it could easily be dismissed. But when dealing with a virus that steals breath from those it infects, where the dominant prescription has been isolation, breathing together creates a life-changing connection for Yang and her patients.
Heart uncentered
After emigrating from Taiwan in the 1970s, Yang’s parents—Christine, an attorney, and James, a physician—settled in Newport Beach, California. As immigrants, they had to adjust their priorities, Yang says, replacing sentiment with success in order to survive—a way of life they instilled in Yang and her older brother as well. “Surviving means having job security, and a title so that you’re indispensable enough to not be marginalized,” Yang says.
Feelings were neither tolerated nor nurtured in her home, so Yang buried hers. She learned to play the role others expected of her as an Asian-American girl, to be “good” and “quiet”—but as a result, an internal disconnect grew: Intellectually, Yang understood her value as a motivated, high-achieving young woman, but she struggled to embody much beyond that emotionally.
At 18 years old, she found herself an anxious, type-A freshman at Barnard College of Columbia University in New York City. She tried a few yoga classes at a friend’s recommendation, but struggled to connect to the practice.
And then, it happened: One day in class, Yang moved into Trikonasana (Triangle Pose). She turned her head to bring her gaze to the ceiling, breathed into the posture, and felt an unfamiliar lightness. A knowing spread throughout her, that she didn’t have to be anywhere or accomplish anything, that she could simply breathe.
“It was the heart expansion,” says Yang, who’s now E-RYT 500 and C-IAYT certified, and who co-authored the book Adaptive Yoga last year. “The actual physical space of my heart, then taking a breath as I expanded the heart and connecting that thought, physical space, and breath. It all suddenly came together.”
At the same time that Yang was exploring this new relationship with yoga, she also developed a bond with her Aunt Shiu-mei, who worked in a lab at Columbia. Shiu-mei brought her niece lunch and helped her with homework. When Yang needed a break from the city, she decamped to Shiu-mei’s New Jersey home for a weekend of cooking, eating, and talking. Where Yang’s parents had been all work and no play, Shiu-mei’s life was full of social outings and travel, of joy and independence. Shiu-mei gave Yang something she hadn’t before experienced—a soft, nurturing kind of love.
Dharma realized
Over time, yoga helped Yang reconnect with the heart she’d been discouraged from nourishing for so long. After completing her yoga teacher training in 2005, she started leading vinyasa classes—something she continued all the way through law school at Duke University and into her first year as a corporate lawyer back in New York City.
In 2005, Yang was 25 years old, making six figures, and killing it by her parents’ standards. But her gut wasn’t sold on this version of success. Then, while in Canada at teacher training, she got a call: Aunt Shiu-mei, who had recently developed idiopathic pulmonary fibrosis—a lung condition that makes breathing incredibly difficult—had suffered a stroke.
Immediately, Yang booked a flight to be at her aunt’s bedside. When Shiu-mei took her final breaths, her niece was there. “Her passing lit both a light bulb above my head and a fire under my ass,” Yang says. Hit by the quickness and fragility of life, she walked away from practicing law, which she’d never truly enjoyed, a few months later. She returned to North Carolina to open a yoga center. “For the first time in my life, I actually followed my instincts,” she says. Her parents looked on in fear, Yang says, believing their daughter was trading in her laudable career to become a gym teacher.
Blue Point Yoga opened directly across from Duke Medical Center in 2006 and was a fast success. The nurses, doctors, and specialists who filled Yang’s classes were curious, posing all sorts of questions about the mechanics of the practice that she didn’t feel equipped to answer. So she researched anatomy and kinesiology in her free time and discussed science in her instruction. Yang loved learning about the intrinsic relationship between yoga and science. She confided in an old friend, who was an oncologist at Duke, that if she could do it all again, she’d be a doctor. “What do you mean, do it all again?” the friend replied. “You’re 27! You still can.” It was all the encouragement Yang needed. In August 2011, Yang entered medical school at Rush Medical College in Chicago.
An inflamed response
The summer of 2020 passed in a haze of disconnect. Uncertainty sat on the shoulder of every decision made, colored by a draining combination of simultaneous information overload and asphyxiation as Yang, in her second year as an attending physician with Sharp-Rees Stealy Medical Group, and her fellow health care workers grasped for any bit of intel that could shift the wind.
Dozens of beds were filled in the COVID unit at Sharp Memorial, hidden behind two sets of doors that Yang could enter only after adorning herself in full PPE. Inside the unit, Yang would stand outside her patients’ doors before entering, watching them gasp for breath, even with the help of a machine. Looking through the door’s window, Yang realized she was mirroring her patients: She had stopped breathing.
Instinctively, her yoga training kicked in. Yang began taking a few breaths to ensure she was present before entering each patient’s room. “Taking this deep breath before I went in was an acknowledgement—that this is really hard, this is all really, really difficult—and then, in that process of caring for myself, being able to let it go and leave it at the door so I could really be there with my patients,” Yang says. It helped. Soon, she wondered whether simple breathing exercises could help her patients, too.
Breathing into Discomfort
COVID-19 starts as an infection in the respiratory system, a nexus that stretches from nose to lungs. Medical experts hypothesize that when your body detects the virus, it reacts with persistent inflammation—a self-healing response that simultaneously throws the body into a constant state of high alert, which in turn wreaks havoc on your organs and tissues, such as those your respiratory system relies on for oxygenation. But yoga practitioners like Yang know there’s a breadth of research to support a different solution.
“Yoga is uniquely suited to assist with COVID-19 recovery,” Yang says. “All the techniques we’re using in pulmonary rehab—comprehensive treatment program for people with acute lung injury—are yoga techniques. We’ve been doing pranayama, we just haven’t been calling it that
Yang is referring to the large body of research supported by the National Institutes of Health on the negative link between yoga and inflammation. A 2012 study, for instance, showed that people with more-regular yoga practices have lower levels of the chemical leptin, which encourages inflammation, and higher levels of adiponectin, which inhibits it. So, Yang hypothesized, yoga ought to be able to help treat the inflammation that causes COVID patients’ most damning symptoms.
When Yang first brought breathing exercises to her COVID-19 patients, she wasn’t intending to treat the virus specifically, but to help her patients feel better generally, to enjoy and benefit from some sense of connection (to Yang, to an activity, to their breath). But the more she incorporated pranayama into her rounds—encouraging her patients to take a mindful pause and a series of deep, diaphragmatic breaths—the more her lens shifted and the practice evolved from an exercise into a protocol. By applying a yogic scope to diaphragmatic breathing, Yang realized she would have two rich bodies of work to reference—her yoga training and her medical training—the marriage of which could guide others in working with COVID-19 long-haulers, as she writes about in the winter 2021 issue of Yoga Therapy Today.
“Diaphragmatic breathing exercises can work to strengthen weak respiratory muscles,” writes Yang about pulmonary complications. “After all, the diaphragm is a muscle, and people often experience global weakness post-COVID. Exercising and strengthening the diaphragm will benefit any postviral syndrome or inflamed physiology. … The primary goal is to strengthen the lungs and their supporting musculature; the secondary benefit is relaxation and activating the parasympathetic nervous system.”
More recently, Yang has been meeting with the hospital’s physical therapists to discuss how to implement the breathing practice more widely, and regularly lectures via webinars to help educate yoga therapists when it comes to aiding their patients with recovery.
Yoga therapeutics for COVID-19 go beyond breathing-related manifestations, Yang says. Movement helps ease vascular blood clots caused by virus-caused tissue damage and inflammation; the lung expansion that comes with Salabhasana (Locust Pose, also called “proning” in the medical field, and a favorite recommendation of Yang’s) soothes musculoskeletal complications; and mindfulness meditation or yoga nidra serves as a powerful therapy for the emotional trauma and disconnect that COVID-19 leaves in its wake.
Underlying each therapy, no matter the symptom or cause, is connection, and in this way, yoga serves one of our most basic human needs.
“In some ways, it’s my job to save lives, which is a little hyperbolic—most days I’m just helping people get through their chronic medical issues. But if I can give them a piece of what saved my life, my self-worth, my heart…” Yang trails off. “We underestimate the degree to which connection and heartfelt love and permission to feel can affect people’s healing, and yoga gave me that permission.”