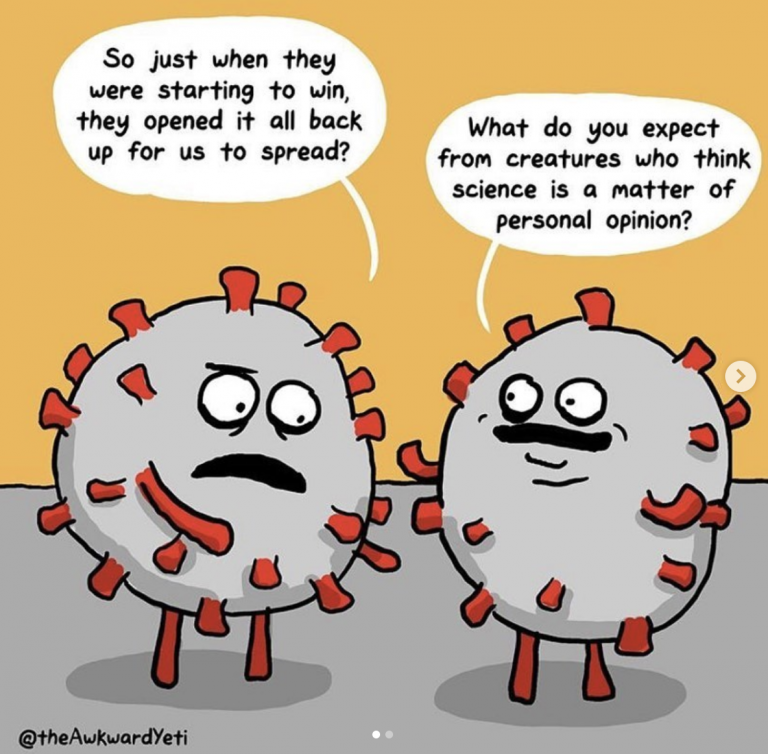
We know how to slow the spread of the coronavirus. And it’s not rocket science. It’s just plain old, run-of-the-mill, everyday science.
Just because our communities and restaurants are opening back up, *nothing* has changed about this virus or its lethality. It can still kill you just as much as it could in March. Maybe there is a ventilator for you now, but there may not be in a few weeks. And for those of my patients that have recovered, most of them have some kind of long-term organ damage – not just in their lungs, but also in their kidneys and hearts. The best thing to do is to not get it.
There is a consistent set of lessons, from around the world, about how to reduce the transmission, and thus your risk, of contracting COVID-19.
The biggest lessons? *Wear a mask if you’re going to spend time near anybody who is not part of your household. *You should minimize your time in indoor spaces with multiple people. *You should move as many activities as possible outdoors. You should wash your hands frequently. *And you should stay home, away from even your own family members, if you feel sick.* The past six months have repeatedly shown the value of these steps. Countries and regions that have taken them have either avoided outbreaks or beaten them back. Over the last few weeks, however, the virus has begun spreading across the southern and western U.S., as well as in some other countries. And there’s no real mystery about why.
The single act of wearing a mask will save lives. Others, and probably yours. And while you’re at it, wash your hands and maintain 6 feet of distance from those not in your household.
Unless you want to end up like one of my patients, who is 33 years old, super healthy, athletic, ran and did yoga every day, and 2 months after recovering from COVID19 (and not even needing to be placed on a ventilator), can still hardly walk 2 blocks without becoming short of breath. Wear a mask for her. Wear a mask for yourself.
Hope this helps and please feel free to share. Love, Dr. Yang
PS: And thanks to @theawkardyeti for the profoundly real and also tragically funny cartoon.